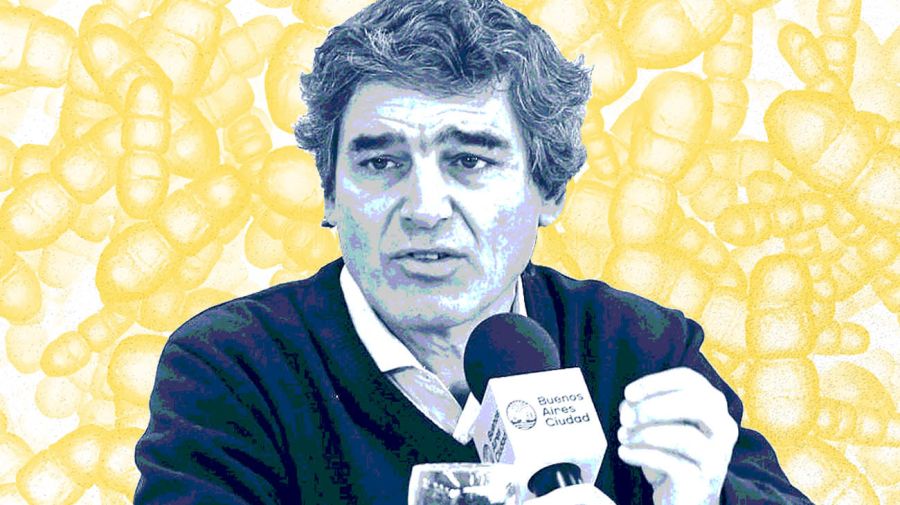
This year there has been more testing than last. What are the most important data to bear in mind – the number of daily cases of contagion, the people in intensive care or the deaths?
All three are important. There are three main epidemiological links, all highly interlinked.
The first is the number of people infected, which is related to the PCR diagnosis, in turn depending on much testing and who is really ill. The City of Buenos Aires has done a lot of work in seroprevalence which has shown that for every positive PCR there are 2.5 people so that we can take that as the ratio for calculating the daily number of the truly ill. It’s a pretty tight ratio even at international level.
From that daily number of the sick we can see since last month a rapid rise which peaked on April 12 at 3,050 cases. As from April 13 (according to the positive PCR diagnoses on that day, not the daily national report) the curve first flattened out and then fell to a daily average of 2,800 cases the following week and then 2,400 the week after. But intensive care beds tend to lag between seven and 10 days behind the curve – in other words, the serious complications develop between seven and 10 days after people fall ill. The curve of intensive care beds thus accelerated in the following week and has flattened out more recently, thus making a future dip sure to come.
The curve of deaths in turn moves between seven and 10 days, on average, after entry into the intensive care ward. The number of deaths has peaked recently in line with the case in question beginning a fortnight or so previously.
There are more intensive care wards. But the cases of older people tend to be resolved one way or another in 10 to 15 days, while the younger can endure up to a month in intensive therapy. Is that right?
Yes. The average age of people in intensive care has gone down in this wave as compared to last winter.
This has to do with a combination of two phenomena. The first is that this wave runs into those aged over 70 and especially over 80 having a very high percentage of vaccination, at least the first dose. This has shown itself to be almost 90 percent effective in reducing the risk of falling seriously ill. Since these age groups are highly protected, they do not occupy much space in intensive care wards, thus naturally lowering the average age. But onto that you need to add this current curve of cases practically doubling last August, which means almost double the number of middle-aged people seriously ill. Naturally the younger the patient, the better their chances of survival and emerging from intensive care in good shape. That’s why people spend longer in these wards.
In the public sector, in collaboration with the private, we work with many wards with a rapid turnover, places with a more intensive and hence faster rehabilitation. That’s how we manage to keep the intensive care beds rotating.
Are we past the peak or will it come in the second half of this month?
We need to be very careful with the curve forecasts and the mathematical projections. They respond on the one side to the natural evolution of the epidemic curve but also to changes in mood and the social decision to be more careful, along with the effects of changes in government policies. Last year we spent all April forecasting the peak for May. When the initial quarantine in Argentina (above all in this City) was so intense, that peak ended up arriving in August.
You have to be very careful when forecasting the peak. One thing is the natural evolution and another what happened in the light of the first restrictions as when all commercial activities and social and family meetings (the prime mechanisms of contagion in this city) were banned, as from the midnight of that first Friday. Then the more recent batch of presidential measures cracking down on nightlife as from 8pm found their response in the curve. Society at large also took the decision to take better care of itself from what it was observing and experiencing. That peak of cases we had on April 12 will probably not return, at least not in the next few weeks.
In the first wave there was great uncertainty because we were totally in the face of the unknown. Today there is more certainty, the health infrastructure is much bigger and nine million people are vaccinated. Why has this second wave hit us so hard?
Everything I say relates strictly to this City, not even the AMBA metropolitan zone since those are the data I know precisely – I like to talk about what I know in detail and where l’m responsible for giving explanations. In the City there is a combination of dimensions which is different in every neighbourhood. That’s why I’m so critical of comparison between countries, provinces and cities.
In the City we had an upsurge after Christmas and during the first half of January. Later those cases fell off but not completely. We were coming off a November floor of 300 cases a day on average and following the upsurge around the turn of the year we moved back to a daily average of some 700. Not only did we take off from a higher floor for the next wave but the level of risky indoor social activities (meetings of families, friends and workmates in homes, offices and workplaces) remained permanent, representing a definite public behaviour. In the City of Buenos Aires the number of cases started shooting up strongly in the March 20 to 30 period when there was not only a certain relaxation of social precautions but also a sudden fall in temperature and several days of rainfall (typical triggers of most autumn waves, according to the European experience). Indoor contacts are really the main risk factor in the pandemic – no face-masks, no social distancing, no proper ventilation in rooms. So the wave took off on the basis of 700 cases a day and a careless citizenry, along with the participation of more contagious variants. But conversely, vaccination has diminished the social transmission of the virus and the health systems have learned how to take better care, which reduced the death rate.
The combination of a declining death rate in hospitals, increasingly contagious strains, less contagion due to vaccination and whether the social mood and weather patterns drive people indoors or out is what determines the evolution of the curve.
There have been surprises like India, whose authorities some months ago were feeling very optimistic and almost declaring the pandemic over, or China, which was exporting its vaccines with only a small percentage of its population vaccinated and is now limiting exports for its use. Is there something going on with this virus which surprises scientists?
I don’t see any concrete surprising data. What is evident, above all in India and other countries in the world and now in the City and AMBA and Argentina, is that there are variants of the virus which are 50 to 70 percent more contagious. Some of them have a certain level of resistance to natural immunity although it’s not that significant – only in the South African variant which luckily has not appeared in Argentina up to now. China took the decision to run a very aggressive vaccination programme for its own protection and India has some intrinsic problems as regards this illness.
We’ve learned from last year, initially in Barrio 31 [a low-income neighbourhood] villa where the illness spread very fast due to the socio-economic difficulties, overcrowding and the habits of sharing. If one person falls sick, the whole family falls sick. In India it has a great deal to do with their culture, their way of life and the socio-economic difficulties.
[Buenos Aires Province Governor] Axel Kicillof has said: “I’m sick of the City saying that it is on a plateau.” Is it really a plateau?
You should never get annoyed over the data of reality because that makes it very difficult for you to cope with it. You need to see the City’s data. Sometimes I say that cases are falling and then somebody comments on the basis of national reports. They are different denominators.
In the City of Buenos Aires, if you take the correct day for the swabs, April 12 was our peak and then the numbers stayed high for between seven and 10 days before coming down appreciably from the previous three weeks. Nothing to get annoyed about and nor are we in a position of leadership to get annoyed. We are where we are to accompany the citizenry, look after it, tell them what we observe and on that basis, propose the best path.

Our metropolis is the third-largest urban agglomeration in Latin America after Mexico City (over 25 million inhabitants) and São Paulo with almost as many while AMBA, has 17 million. The authorities in both inner and outer São Paulo come from the same party while Mexico City is a single political unit, the Federal District. But of the 17 million inhabitants here, three million live in the City of Buenos Aires while the other 14 million are in Greater Buenos Aires. Does that make public health harder to manage?
It adds a certain complexity but that’s why we are in office, to build bridges. They are two different things. I speak of the City’s data because I know them and have to answer for them, which does not mean that I fail to understand that there is a broadly similar behaviour across the urban agglomeration, especially in the inner belt of Greater Buenos Aires, closely linked to our city.
From the outset we have defended the need for cooperation, collaboration and a common strategy for AMBA with the national government and both the national and provincial Health Ministries – we do so permanently. We have to propose a common path to the citizenry while understanding that there are variants or particular features of the City and Greater Buenos Aires which sometimes require a tactically differentiated implementation on both sides. Greater Buenos Aires has heavy industry while the City of Buenos Aires is more commercial. We three ministers have followed a strategy of cooperation, collaboration and a common outlook. Sometimes there is a certain level of divergence in public and political statements but that does not occur in daily practice.
Are private healthcare providers closer to the position of Buenos Aires Province?
These have the difficulty of their subsystem having a certain level of rigidity to share general resources – that’s why it’s natural to be a bit more worried. Their subsystem is metropolitan by definition with their coverage having partners throughout AMBA but centred above all in the City of Buenos Aires. They have practically 40 percent of the intensive care beds occupied by citizens of Buenos Aires Province so you cannot just look at it from a City standpoint.
As for the request for measures, you have to look at that in a bit more detail, explaining to people what is going on and agreeing on a roadmap with the citizenry – a roadmap which also means every citizen contributing something. Any measures are useless if people see them as insufficient or unfeasible – the latter generate very much more tension in society. For every epidemiological situation we propose a package of measures geared to that situation but concretely trying to cut the mechanism of contagion. In the City we saw the main mechanism of contagion as indoor meetings (both for work and social purposes) and in nightlife, scorning protocols. When those two decisions were taken, the curve began to dip.
You need to be precise about where contagion is occurring and up to what point the citizenry is ready to accompany you and what it is capable of doing. We seek to do everything with as little social pain as possible. We’ve been going for more than a year now and people have been losing their capacity to accompany us.
Does the minister Carla Vizzotti listen to you?
We have permanent dialogue. We had it with [former Health minister] Ginés [González García] and we have it with Carla. We health experts have the outlook that these issues require cooperation while the federal model obliges us to adopt that form of management. In the pandemic there is no room for anything else. Then, as always, we can have subtly different interpretations because we look at the City’s specific data while the national Health Ministry looks at Argentina as a whole. Then we might have some divergent outlooks as to implementation but all within normal dialogue.
Peronism boasts some highly recognised health experts like Ginés himself, while the Radicals can always point to Arturo Oñativia. PRO is a young party, does it have its own school of health?
Yes, we approximate the others with a different outlook but in public health the margin of differentiation is relatively narrow. Both sides of the ideological and political spectrum share a relatively common outlook on public health with styles and subtleties. Peronism has a long track record, as does Radicalism while our Cambiemos coalition implies a joint outlook – that‘s the road we’re building. The definition of style is in the construction.
[National] Health Ministry Cabinet Chief Sonia Gabriela Tarragona was previously director-general of the Mundo Sano foundation and co-founder of Grupo Insud [headed by Hugo Sigman]. Minister Vizzotti directed and taught the master’s degree for pharmacological policy at the Universidad de Isalud [also founded by Ginés]. Does any equivalent of this grouping exist among the Radicals or Juntos por el Cambio?
Ginés was a great team-builder in Argentina. He has a long track record. He built up an academic-political university. Among Radicals Aldo Neri was a great leader but that construction continues to evolve in the form of political participation.

Is it correct to say that Argentina’s current vaccine problem is named AstraZeneca?
That seems to me to be straining reality a bit. Argentina is embedded in a world with serious difficulties in meeting delivery commitments – practically every company has run into difficulties. Argentina’s strategy was grounded in two major manufacturers: the Russians [Ed. Gamaleya Institute] on one side and AstraZeneca on the other. We had difficulties with both. While the component of Sputnik V came closer to meeting commitments, there were also delays which were much bigger with AstraZeneca. Both main pillars of the contract had difficulties, you cannot just point to one.
Why did the word “negligence” end up being something which impeded negotiations with Pfizer while there was no problem with other United States and European vaccines ?
I have no precise knowledge of those negotiations nor whether that word was the entire problem. I cannot answer that. Every company will have made its own evaluation of the risk and will have entered into dialogue. You and I are talking about a whole bunch of meetings, documents, agreements and disagreements which we do not know in detail.
Are some labs stricter than others and is that usual in the vaccine world?
This pandemic has changed all the conditions of daily reality. If you read the Argentine law on the purchase of vaccines outside the context of this pandemic, you would say: “That’s inadmissible.”
Is it too soft on the labs?
Yes indeed. A law to purchase any medical input under these conditions is inadmissible. But when you look at the scenario within which that law was approved, you’d say: “In this scenario that risk may be taken.” That’s the debate. Nations were asking to contract the purchase of vaccines which had not even completed their clinical research so that nobody could say with any precision what the risks were, even after Phase 4. You were asking for the deliveries of vaccines when even their producers could not give their word as to its effects. The first contracts were made as from last July when Phase 3 had only just started. The health emergency, the worldwide catastrophe led to an acceleration of production, research, contracts and delivery commitments. That was the context in which the debates between countries and companies must be placed, also in Argentina. It’s not a normal debate – the situation is absolutely abnormal.
Some 80 percent of the vaccines received by Argentina come from Russia or China. Is that also abnormal in the vaccine world?
The proportion of vaccines received by Argentina is very different from most Western countries. Most of those countries made contracts with private companies, especially from Europe and the United States. Argentina launched a massive contract with an Anglo-Swedish company and then brought everything from the states offering the most rapid response at that time. I’m speaking of an average because there were other countries buying vaccines in a fashion similar to our own.
To what do you attribute countries like Russia and China only vaccinating a small percentage of their population and then exporting vaccines?
Such opinions often come with scant data and without details. My opinions on other jurisdictions or countries are always very prudent for that reason. The Chinese and Russian scenarios seem very different to me. If you look at the pandemic at the global level, you will note that Southeast Asia and Oceania reacted to the pandemic in a way extremely different from Europe and the Americas, leaving aside the African continent with its own very particular features. Southeast Asia and Oceania had a far milder experience. Some assume that this was because of the political decisions they took; others think that it was because of different biological conditions.
As a health expert, do you feel frustrated to see how public health issues have become politicised in certain countries?
“Frustrated” wouldn’t be the word. There is an imperious need for individual and collective reflection. I often talk to my team about the painful contexts which are so difficult to avoid. But any painful situation also carries with it a first moment of taking care, accompaniment and empathy. Every situation in the individual and collective life of peoples has to lead to a profound reflection on how we got there, how that context was built up and how we could undergo it as a community so that nobody is left out or in the worst position.
I have the feeling that we still have not been capable of understanding this opportunity and facing it as a possibility to move ahead as a society while understanding that divergences and differences are part of what makes us a people and not a social problem. They represent who we are as a community. Out of that diversity, those individualisms, those subjective viewpoints must arise a collective proposal which transcends them. It may become a lost opportunity if we do not know how to administer, evaluate and reflect on it with appropriate dialogue.
Brazil has its own Instituto Butantan and is thinking of manufacturing a million vaccines a day and 100 million in the first year against coronavirus. It depends on São Paulo, not their national government which then says that it will not approve the Sputnik for lack of information when the Chinese vaccine has published even less information than the Russian. Even when approving vaccines, is there more politics than public health?
This is an illness which has altered every dimension of the human being – not only public health, the socio-economic and personal relations but also decision-making and power.
As a health expert I see political participation as profound. Party politics, which is less transformational, is the big problem of the pandemic. We must not accept ideological or partisan outlooks marking distances in our capacity to tread a common path. Your example is concrete. Unfortunately neither national nor local leaders have been capable of treading a common path and that is something which might also happen in our community.
Is your surname Quirós or De Quirós?
My surname is actually González Bernaldo de Quirós. It’s complex, typical of Spanish immigrants, partly coming from my father and partly from my mother. I’ve simplified it because such a long and cumbersome surname has caused me many problems of identification and almost a split personality.
The opinion polls point to you as the best parliamentary candidate for Juntos por el Cambio in the City for the October midterms but it would be untimely with the battle against the pandemic. Would you accept being a candidate in 2023?
I don’t know what I would accept tomorrow at this stage of my life. Until a couple of years ago I had had 30 years of professional development at the Italian Hospital, a non-profit hospital.
At that stage of my life at the age of 57, turning the corner in such a definite manner, I had the feeling, the conviction, the inner sureness that then was the time to return to society what it had allowed me to construct, which is what I am doing now. I went to a public university because I had no other possibilities. Medicine rescued me, gave me the possibility to develop both professionally and economically. I never imagined that it would be such a profound, intense and difficult effort.
I don’t know how much energy I’m going to have in the future. From here to 2023 is what comes next. In all honesty I cannot answer you but what I do want to say to the people is that I’ve come to give. I’ll give it all I’ve got, without holding back anything.
Most politicians are lawyers, economists and engineers. What can doctors contribute to politics?
Doctors have different talents to contribute and being complementary is always necessary. What I would most like to contribute is that capacity of empathy along the lines of the doctor/patient relationship, understanding the outlook of other people.
It is possible to return to politics with a capital “P.” In the modern world the paternalistic and authoritarian politics of governments deciding for the people are out of date. Society needs people who can understand, who can make and receive proposals, capable of constructing a path horizontally. Passing from paternalistic politics to consensus.
Have you ever asked yourself if this pandemic might not be a sign of something more?
I did not feel so much the obligation to dedicate myself to public life as an inner conviction. There’s a subtle difference. Life has infinite paths to discover and travel. I see no advantage in being better-known, it was one of the consequences of this path in life. I have to be up to what the citizenry needs and expects of me. If that transforms itself into a value, I’ll go discovering that along with other people.
I’m not going any place, I’m just travelling where I wanted to go. The process is more important than the destination and I’m in this process with enormous difficulty, pain and fatigue but with the inner conviction that this is the path I had to take.


















Comments